By Rebecca Finkel
The Big Picture: COVID Rates Rising in the South
As of this posting, the CDC is reporting a total number of 6,181,474 COVID-19 cases in the country, which is an increase of 290,942 in the past seven days. California, Florida and Texas still lead the country in total cases, but case rates (# of infections per capita) are highest in the Southeast part of the country, the highest being recorded in Louisiana, Florida, and Mississippi. Louisiana reported 5,425 new cases in the past seven days, which brings the state’s current rate to 3,270 cases per 100,000 residents.
Introducing The PPE Storage Index
This past Wednesday, Get Us PPE rolled out our PPE Shortage Index, which will offer a monthly update on the national PPE shortage based on the data we receive as the largest non-governmental distributor of PPE. This data will track national, regional, and state-specific PPE-related data, such as the number of requests by state, items most requested, and supply remaining by type. It can also inform future models for equitable distribution of PPE and other supplies during a disaster, such as treatments or vaccines.
Key Data Takeaways: August 2020
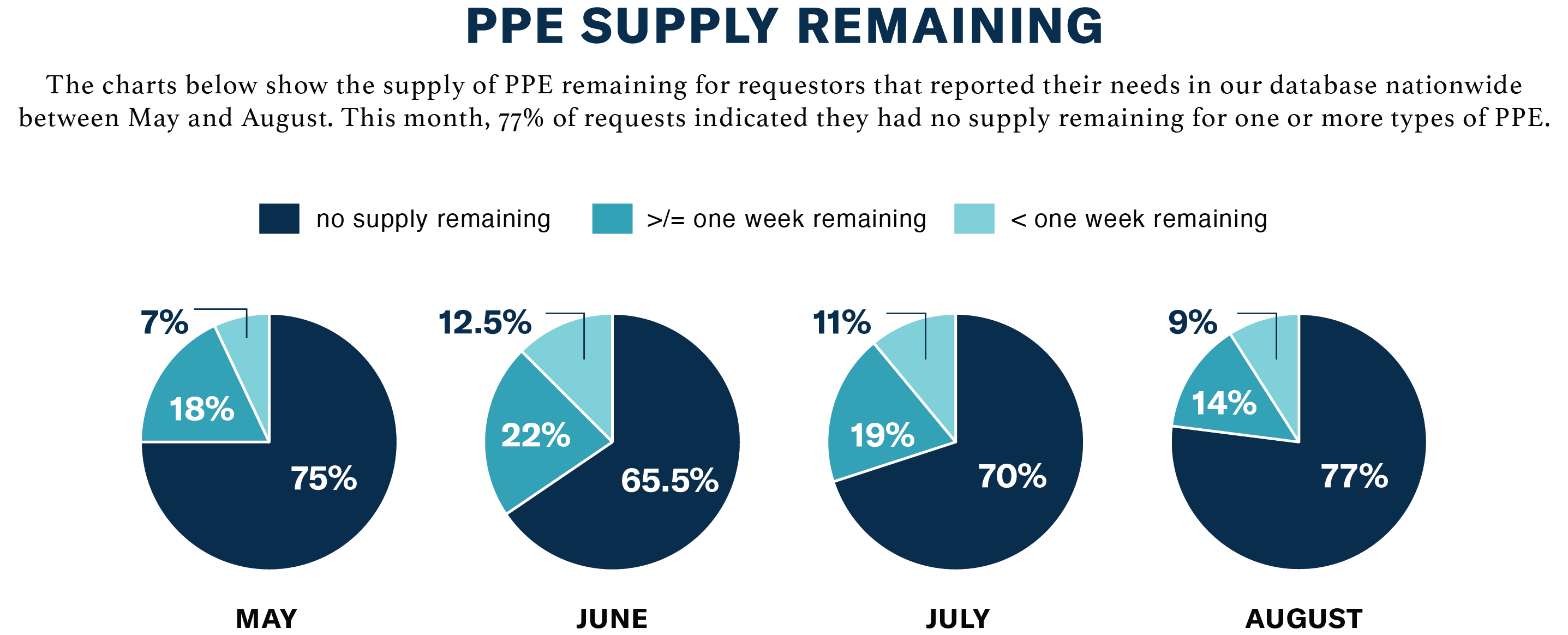
- The U.S. still faces serious PPE shortages; 77% of facilities who requested PPE report having no supply left of one or more types.
- While large hospital systems are beginning to benefit from a recovering PPE supply chain, smaller, non-hospital facilities still face acute PPE shortages.
- There is a strong correlation between PPE requests submitted to Get Us PPE and new COVID cases reported per state in August.
Download the full Get Us PPE Shortage Index >
The Cost of the Crisis
On Tuesday, the Congressional Budget Office projected that the federal budget deficit would reach $3.3 trillion in 2020, due in part to economic disruption caused by the pandemic. A Joint publication released this week from UC Berkeley School of Public Health and UC Berkeley Labor Center, Economic and Health Benefits of a PPE Stockpile offers insights into how PPE shortages harmed California’s population and economic health, and how this phenomenon may have played out across the country. The researchers found that “Procuring an adequate PPE stockpile in advance at non-pandemic prices would cost only 17% of the projected amount needed to procure it at current pandemic-inflated prices.”
In California, an inadequate PPE stockpile led to:
- Inflated PPE prices. For example, New York State paid $7.50 for each N95 mask, which usually cost $1/each. The federal government reportedly paid six times the pre-pandemic cost for N95 masks, plus increased costs for expedited delivery.
- Increased unemployment payments of approximately $93 million, due to lack of PPE
- An estimated 20,860 COVID-19 infections among essential workers.
Consistent with findings from our PPE Shortage Index, which registered a total of 3,103 requests from California facilities since March, the report cites a California Health Care Foundation survey of skilled nursing facility staff in which more than 20% of respondents reported not having enough PPE. 80% reported being very or extremely concerned about contracting COVID-19 at work.
FEMA to Cease Funding PPE in Schools
Although federal guidance recommends masks for face-to-face teaching, the Federal Emergency Management Agency (FEMA) announced on Tuesday that it will no longer reimburse states for the cost of supplying PPE in schools. Other federal assistance will be available to distribute cloth masks for schools, including an effort by the Department of Health and Human Services to allocate a total of 125 million cloth face masks for use by teachers and students. The number of masks available to each state will depend on that state’s number of low-income students. While this distribution effort aims to be equitable, it is yet to be seen if the measure is sufficient to provide adequate PPE to schools in need for the duration of the crisis. The cancelation of FEMA’s plan could leave many teachers seeking other avenues to defer the cost.
Child care centers are feeling a similar pinch. These facilities, which already suffered due to closures in the spring and the decreased enrollment that followed, now face largely increased operating costs in order to keep students and teachers safe. This week, new reporting by the Center for American Progress broke down these costs and found that “providers are facing, on average, a 47 percent increase in operating costs during the pandemic, with even higher increases for programs serving 3- and 4-year-olds.”
Licensed centers must follow stringent sanitation guidelines to remain open, which require the purchase of additional cleaning equipment (now, on average, 12% of a facility’s total operating budget) other equipment, such as non-contact thermometers, staffing to accommodate student-to-teacher ratios, and, of course, PPE. Initial CARES Act funding of $3.5 billion is predicted to be insufficient to offset these costs, and additional funding of $50 billion, passed by the House, has stalled in the Senate.
Aside from the importance of protecting the health of staff and children, safe and functional childcare centers are crucial for allowing essential workers to do their jobs. There is a deep economic and social impact when child care is not available, mostly to women and communities of color. In response to this growing need, Get Us PPE will soon launch a new initiative, PPE for Schools, as well as a focused donor fund to help get donated PPE to the schools that need it most.
Get Us PPE In the Media
Co-founder Megan Ranney lent her expertise as a physician and a parent to the New York Times in the article, A Parent’s Toughest Call: In-Person Schooling or Not? Dr. Ranney emphasized the importance of the use of masks by children when participating in in-person school or other indoor activities.
“I will not send my children to school or to an indoor activity where the children are not all masked,” Dr. Ranney said.
The launch of the PPE Shortage Index was featured in Yahoo Finance and MarketWatch, among others. Media inquiries can be sent to Amanda Peery-Wolf, PR Manager, and Stephanie Zeller, PR & Data Visualization Strategist, at media@GetUsPPE.org.




