By Angelika Pavlovna
In the global fight against COVID-19, healthcare professionals are seeking the best protection available. The two primary medical-grade PPE products that cover the mouth and nose are N95 respirators and ear-loop surgical masks. Both the N95 and the surgical mask are designed for single-use purposes, and are intended to be thrown out if they become contaminated, deformed, soiled, or improperly fitted. While N95 respirators and surgical masks both create an important barrier, their usage and level of protection differ significantly.
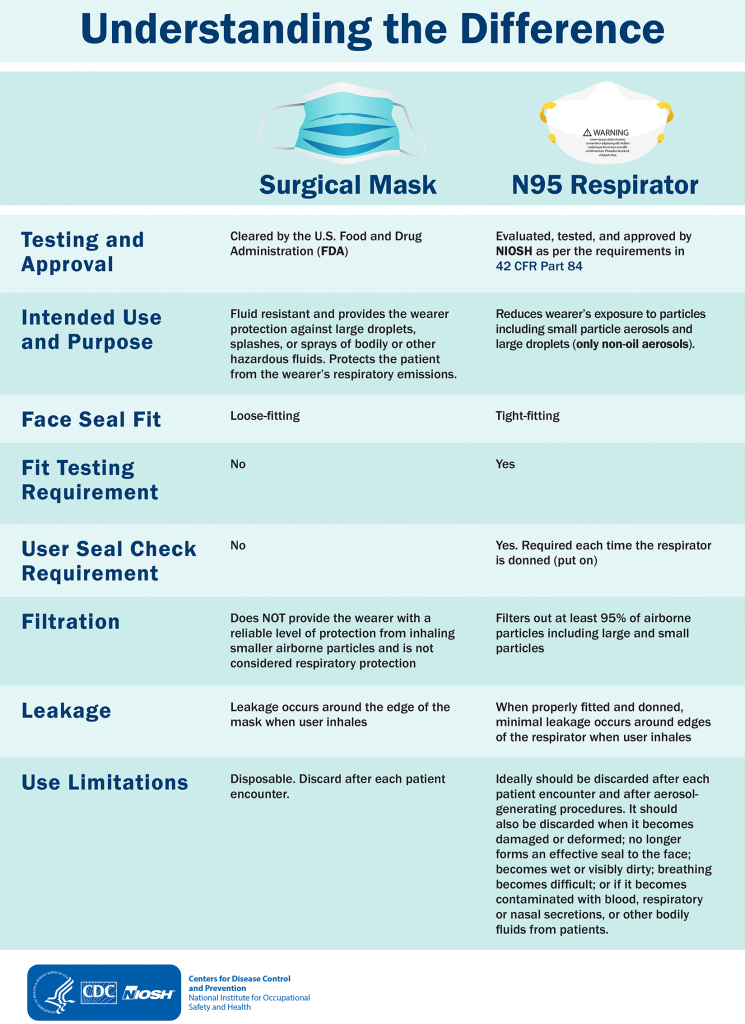
Surgical masks, also known as medical or procedural masks, are typically constructed with micro- and nano-fibers to create a three layer, non-woven fabric barrier. Depending on the model, many incorporate pleats to allow for protection over a greater surface area, with ties or ear loops included to hold them securely in place. Surgical masks are primarily used during non-aerosol-generating procedures (such as routine clinical work) to prevent the wearer from inhaling larger droplets and particles—which may contain harmful bacteria or viruses, including COVID-19. They also work to prevent particles released from the user from contaminating other individuals or falling on nearby surfaces. They are not designed to fit with a tight seal, and therefore, cannot entirely protect the wearer from all particles, such as those released during aerosol-generating procedures.
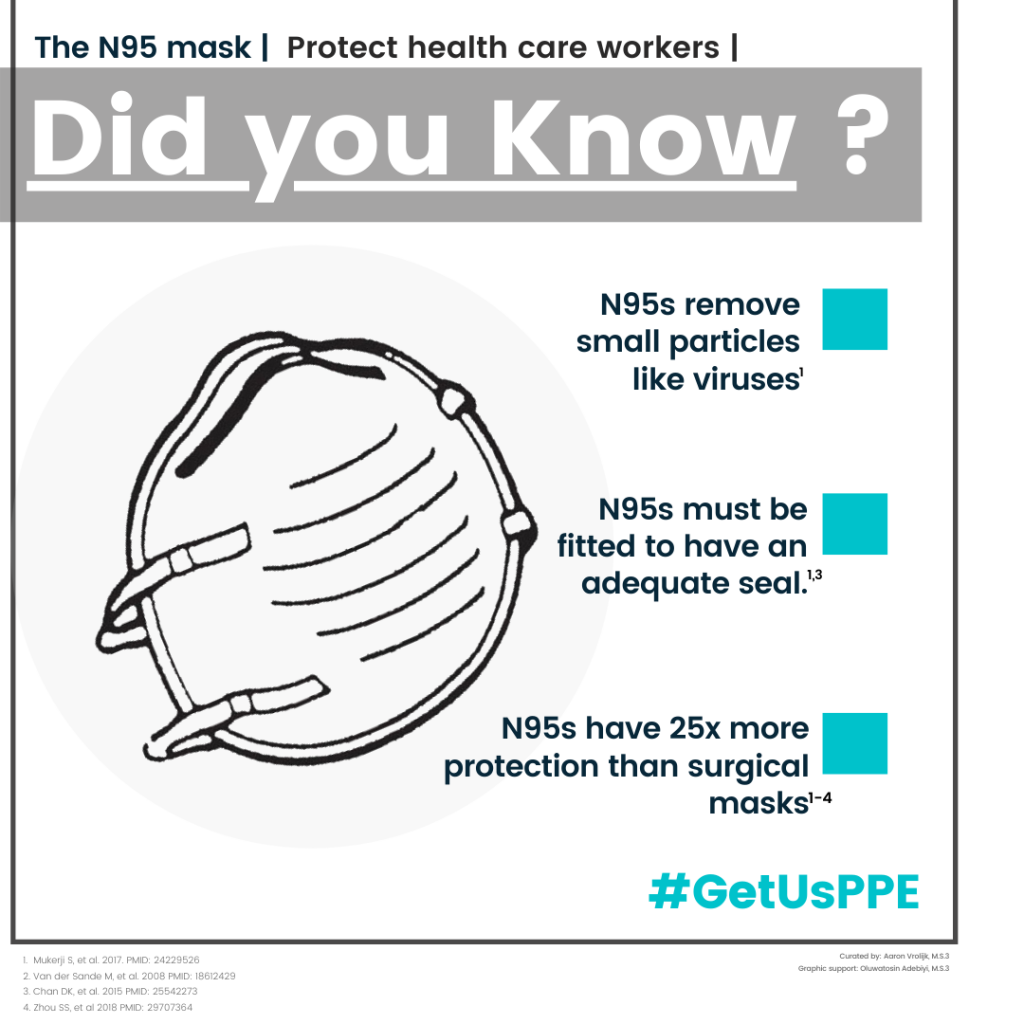
An N95 respirator, in contrast, encloses the mouth and nose in a tight seal, offering the highest amount of protection from potential airborne particles. When properly fitted and attached, an N95 respirator can filter out 95% of small airborne particles (0.3 micron). The technology behind the N95 involves a network of electrostatically-charged polymer fibers, which acts as a filter to trap incoming particles such as dust, pollutants, and viruses. Overall filtration capabilities actually increase over time—once trapped, these particles help to filter out more incoming particles—but breathing tends to become difficult after eight hours of use, as the respirator’s fibers become too clogged to allow for proper inhalation. While it is crucial that a N95 respirator is properly tested and fitted, a surgical mask is generally manufactured in one size. The manufacturing of N-95 respirators is regulated by the National Institute for Occupational Safety and Health (NIOSH), while the production of surgical masks is approved by the US Food and Drug Administration (FDA).
 The Center for Disease Control (CDC) is currently encouraging the public to wear homemade, cloth face masks, in order to conserve N95 respirators and surgical masks for healthcare professionals as both forms of medical-grade PPE are in extraordinarily high demand. Unlike an ear-loop surgical mask, a cloth mask is not approved to protect its user from microscopic airborne pathogens, but is nonetheless thought to serve as a valuable preventative measure, preventing those who may be sick (or asymptomatic) from spreading the virus to others.
The Center for Disease Control (CDC) is currently encouraging the public to wear homemade, cloth face masks, in order to conserve N95 respirators and surgical masks for healthcare professionals as both forms of medical-grade PPE are in extraordinarily high demand. Unlike an ear-loop surgical mask, a cloth mask is not approved to protect its user from microscopic airborne pathogens, but is nonetheless thought to serve as a valuable preventative measure, preventing those who may be sick (or asymptomatic) from spreading the virus to others.
A 2015 study in 14 secondary-level and tertiary-level hospitals in Hanoi, Vietnam compared cloth and surgical mask’s efficacy. Different hospital wards were designated to wear surgical or cloth masks while other wards proceeded with their normal practices (the control group). The test subjects wore their individual cloth or surgical mask for four weeks throughout their shifts. Many of the participants concluded with respiratory virus infections and influenza-like illnesses (ILI), especially those who had worn a cloth mask. The study found that “Penetration of cloth masks by particles was almost 97% and medical masks 44%.” Both masks demonstrated that re-use, substandard filtration, and moisture retention led to an increased chance of infection.
In another study performed by the Shanghai Jiao Tong University School of Medicine, the surgical mask used in an occupational setting became increasingly contaminated the longer a surgeon wore it. The interior layers of the mask picked up more bacteria from its user than from its external environment. The study concluded with a recommendation that surgical masks in medical environments should only be worn for two hours before users don a new, sterile one. In addition, surgical masks with thicker filtration or multiple layers are potentially more effective.
Surgical masks are a critical piece of personal protective equipment in the efforts to slow the spread of COVID-19. While the masks do not provide a reliable level of respiratory protection, their resistance and filtration is extremely effective in shielding both patients and healthcare providers for a limited period of time. The sooner we can provide this essential gear to our healthcare workers, the safer they will be in aiding others.