By Dana Glaser
Since the CDC issued guidance three weeks ago that Americans should wear face masks in public to prevent the spread of COVID-19, a lot of people have been scrambling to get clear on the difference between different kinds of masks, how they work, and who should wear which masks, when. This post explains the differences between your new favorite dinosaur-printed mask and the face coverings we desperately need to supply healthcare facilities, the much-discussed N95 respirators, and everything in between. Using the right mask in the right situation can help ameliorate the risk posed to healthcare workers by the dire shortage of medical grade respirators.
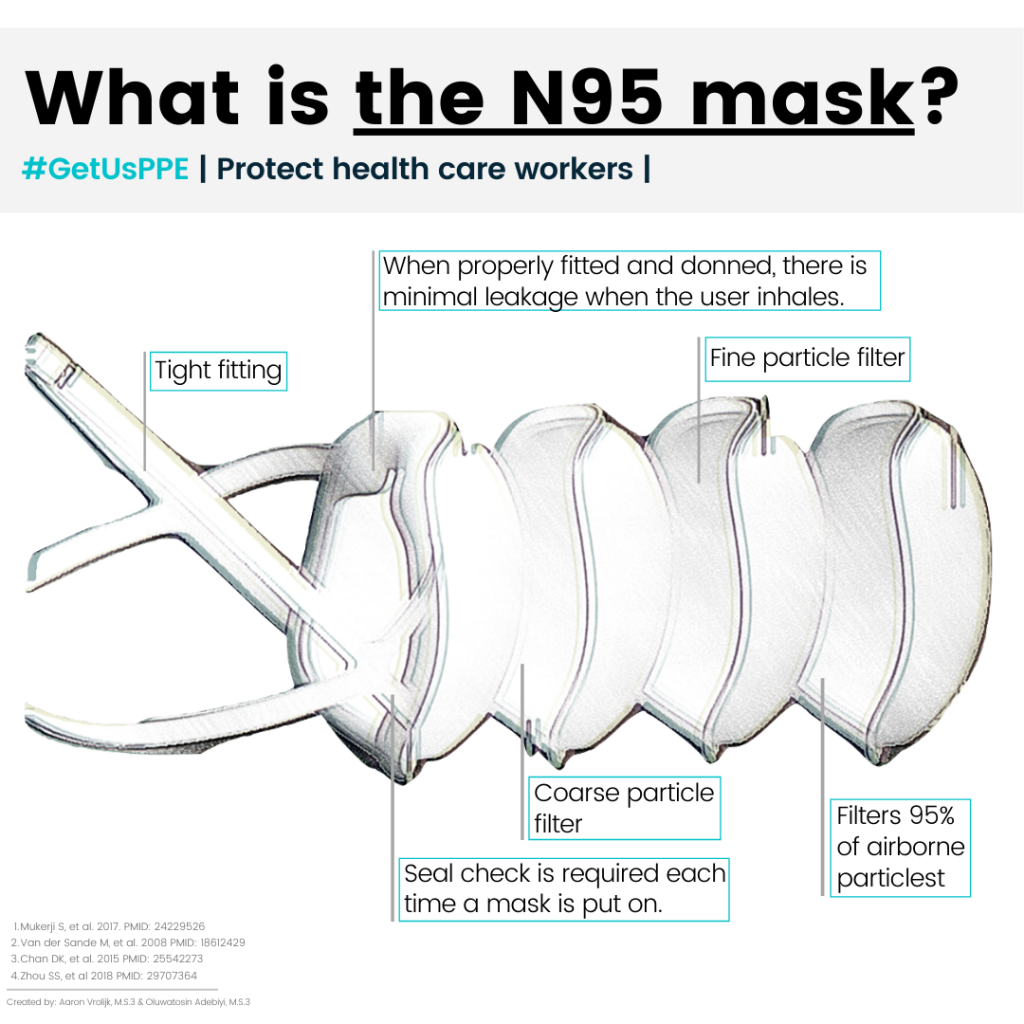
N95 masks are technically not masks: they’re respirators, or more formally FFRs (Filtering Facepiece Respirators). Unlike cloth procedure masks, which loosely tie at the back of the head or loop over the ears, N95s are designed to seal off the nose and mouth by closely fitting to the face. They’re made from materials that have the ability to filter out small particles from the air; so where procedure masks protect the wearer and those around her from larger droplets, respirators also protect the wearer from much smaller particles that linger in the air (the dispersion of these much smaller particles is called aerosolization). Because of the specificity of the filtration materials and the need for close fit, N95 respirators are difficult to manufacture.
N95 is a designation made by NIOSH[1] (National Institute for Occupational Safety and Health) that refers to the percentage of airborne particles the respirator filters out when the wearer breathes. The N95 filters out 95% or more airborne particles; it is the lowest of 7 designations made by NIOSH for FFRs (i.e, the N99 filters out 99% of airborne particles). NIOSH approves respirators for use in a variety of occupational settings, like construction sites; a surgical N95 mask refers to a subset of N95 models that have also been approved for surgical use by the Food and Drug Administration. Different countries have different standards for approving respirators for medical use; designations such as KN95 and FFP2 refer to respirators similar to N95s approved for certain performance standards in other countries (China and Europe respectively).[2]
 Under circumstances in which there is no supply shortage — a situation already largely imaginary for many hospitals at this point — the CDC recommends surgical N95 respirators for healthcare personnel who need protection from both airborne and fluid hazards, like splashes and sprays. In times of shortage, they suggest only HCP working in sterile fields who need protection from airborne and fluid hazards should wear surgical N95 respirators. Other healthcare personnel may wear standard N95 respirators, and if there is a risk that those HCP may be exposed to sprays and splashes, they can wear N95 respirators with a face shields over them.[3] Here’s a nice illustration of the preferred versus the merely acceptable situation. This guidance assumes that N95s are being used in settings, like hospitals, that already comply with OSHA’s regulations for respiratory protection.[4] Medical professionals have to be trained to identify situations in which respirators are necessary, and N95 respirators have to be fit-tested on healthcare professionals annually. According to the CDC, then, it’s not currently possible to effectively use respirators in settings like nursing homes and outpatient clinics that don’t have respiratory protection programs in place.[5]
Under circumstances in which there is no supply shortage — a situation already largely imaginary for many hospitals at this point — the CDC recommends surgical N95 respirators for healthcare personnel who need protection from both airborne and fluid hazards, like splashes and sprays. In times of shortage, they suggest only HCP working in sterile fields who need protection from airborne and fluid hazards should wear surgical N95 respirators. Other healthcare personnel may wear standard N95 respirators, and if there is a risk that those HCP may be exposed to sprays and splashes, they can wear N95 respirators with a face shields over them.[3] Here’s a nice illustration of the preferred versus the merely acceptable situation. This guidance assumes that N95s are being used in settings, like hospitals, that already comply with OSHA’s regulations for respiratory protection.[4] Medical professionals have to be trained to identify situations in which respirators are necessary, and N95 respirators have to be fit-tested on healthcare professionals annually. According to the CDC, then, it’s not currently possible to effectively use respirators in settings like nursing homes and outpatient clinics that don’t have respiratory protection programs in place.[5]
The CDC has essentially ranked the kinds of trade-offs hospitals can make in order to preserve supply of N95s and use limited supplies most effectively as the situation deteriorates from “preferred” to iterated degrees less than really acceptable. Preferred options include using NIOSH approved alternatives to N95s where possible; all of these alternatives provide protection equal to or better than the N95 respirator. They are NIOSH approved FFRs (such as N99, N100), elastomeric half mask and full facepiece air purifying respirators, and powered air purifying respirator (PAPRS). Less preferred alternatives, in descending order, include: extended use of some N95 respirators; using N95s that have exceeded their shelf-life in procedures, and limited re-use of N95s (taking it off and putting it on again ). The CDC has a useful chart outlining just how much PPE a doctor should don in true scarcity given just how much proximity to a patient they plan to engage in, and just how much PPE that patient can be wearing him or herself.
The CDC also advises prioritizing the use of respirators by the type of procedure or activity being performed. In very general, this means that healthcare personnel should, according to the CDC, be wearing face masks at all times while in the healthcare facility, but might switch to respirators when they’re directly treating COVID-19 patients and PPE is required. This is where the humble “cloth-covering” we’ve all been trying to learn to sew makes its re-entry onto the scene: it’s not always easy or possible to tell exactly when PPE is required. Patients come into the hospital with COVID-19 who have not yet been diagnosed. Asymptomatic visitors come to see grandparents with heart disease. Having every patient and visitor wear a “cloth-covering” helps limit the risk doctors take when healthcare facilities have to limit the use of N95s to direct contact with COVID patients.
[1] https://www.cdc.gov/niosh/npptl/topics/respirators/disp_part/. On this page you may also find a list of all 7 of NIOSH’s FFR designations, and a list of N95 manufacturers organized alphabetically.
[2] A useful comparison of the differences between different performance standard designations in different countries can be found in this Technical Bulletin from 3M, a NIOSH approved manufacturer of N95s.
[3] https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/index.html
[4] https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.134




