Personal Protective Equipment (PPE) have become an emblem during the fight against coronavirus. Like masks, gowns and coveralls are identified as critical components of isolation precautions against harmful pathogens. As the number of COVID-19 cases grow tremendously in the United States, the demand for PPE increases.
By Zayba Syed
WHY PROTECTIVE GARMENTS?
Healthcare workers wear protective garments to prevent the transmission of microorganisms. The Centers for Disease Control and Prevention have designated three routes of transmission.
-
CONTACT – DIRECT (PHYSICAL CONTACT)/INDIRECT CONTACT (CONTACT WITH A CONTAMINATED SURFACE) BETWEEN AN INFECTED PERSON AND SUSCEPTIBLE PERSON THROUGH THE SKIN AND MUCOUS MEMBRANES (EYES, NOSE OR MOUTH)
- PPE REQUIREMENTS: GOWN AND GLOVES
- TO REDUCE TRANSMISSION: DISINFECT FREQUENTLY TOUCHED SURFACES, WASH HANDS AND WEAR PPE
-
DROPLET – TRANSMISSIONS PASSED THROUGH SNEEZING, COUGHING OR TALKING
- PPE REQUIREMENTS: MASK, GOWN, FACE SHIELD/GOGGLES AND GLOVES
- TO REDUCE TRANSMISSION: WEAR PPE AND WASH HANDS
-
AIRBORNE – TRANSMISSION PASSED THROUGH MICROORGANISMS SUSPENDED IN THE AIR (DUST PARTICLES AND AIR) THAT ENTER THE RESPIRATORY TRACTS
- PPE REQUIREMENTS: N-95 MASK, GOWN, FACE SHIELD/ GOGGLES AND GLOVES
- TO REDUCE TRANSMISSION: WEAR PPE, DISINFECT SURFACES AND WASH HANDS
According to The World Health Organization, COVID-19 is transmitted from person to person through droplets in the air created by an infected individual breathing, sneezing or coughing. These droplets can reside on surfaces for long periods of time. Consequently, a healthy person can contract the virus through cross-contamination when touching this infected surface before touching their eyes, mouth, face or nose. Frequently disinfecting surfaces and washing hands will help reduce contaminants. Additionally, people can become infected by inhaling droplets in the air created by infected individuals. Therefore, maintaining social distance and staying 3 feet away from others is important to avoid transmission of COVID-19.
HOW DO PROTECTIVE GARMENTS PREVENT THE MOVEMENT OF MICROORGANISMS?
Microorganisms of various sizes can survive traveling large distances and under extreme conditions. When designing a gown, the integration of fabric, comfort, functionality, durability, coverage, viscosity and relation to biohazard controls are all taken into consideration. Standardized test methods (ANSI/AAMI PB70 Standard) are used to detect penetration. The test includes four standards, Impact Penetration, Hydrostatic Pressure, Synthetic Blood Penetration and Viral Penetration Test. Specifically for isolation gowns, the more comprehensive ASTMF1671 Viral Penetration Test is administered. American Society for Testing and Materials (ASTM) International has provided standard tests specific to COVID-19 here.
American Society for Testing and Materials (ASTM) International COVID-19 Test Standards: https://www.astm.org/COVID-19/
TYPES OF PROTECTIVE GARMENTS: COVERALLS VS. GOWNS

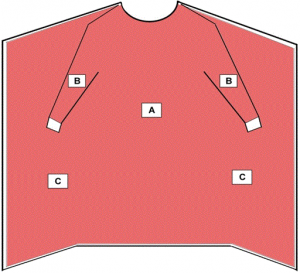
Coveralls and gowns have been used in the healthcare field as effective garments to prevent the spread of microorganisms. Traditional isolation gowns are more commonly utilized and therefore more healthcare workers are familiar with proper techniques on donning (wearing) and doffing (removing). It provides partial coverage with back and mid-calf openings. Coveralls provide full-body coverage (sometimes including the head and feet). Seams/closures within coveralls are important components that also amount to the durability and effectiveness of the garment.
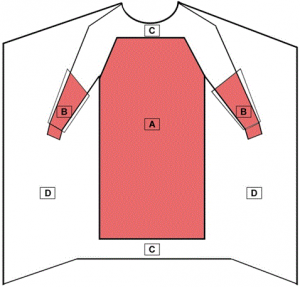
CRITICAL AREAS
According to the Food and Drug Administration, typically, the highest areas of exposure of contaminants during a surgical procedure include the chest and mid-arm region and below. When in an isolation room, all areas of the gown are susceptible to exposure.
THE CDC RECOMMENDS LOOKING AT THREE FACTORS:
- ANTICIPATED EXPOSURE AND PURPOSE OF USE
- DURABILITY, APPROPRIATENESS AND MATERIAL PROPERTIES
- FIT AND STERILITY
HOW DO I WEAR A GOWN: DONNING (WEARING) AND DOFFING (REMOVING)
DONNING
STEP 1: UNFOLD GOWN AND PLACE ARMS THROUGH EACH SLEEVE
STEP 2: TIE THE NECKBAND AND WAISTBAND
STEP 3: WEAR GLOVES (STRETCH GLOVES OVER WRIST AREA OF THE GOWN)

DOFFING
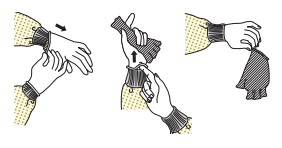
STEP 1: BEFORE REMOVING GOWN, REMOVE ONE GLOVE AND HOLD IN GLOVED HAND
STEP 2: SLIDE FINGERS OF UNGLOVED HAND UNDERNEATH THE CUFF OF THE REMAINING GLOVE AND SLIDE THE GLOVE OFF TURNING IT INSIDE OUT (TO AVOID CONTAMINATION)
STEP 3: DISCARD GLOVE
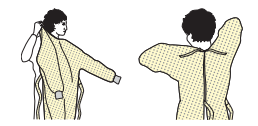
STEP 4: UNFASTEN TIES AT THE WAIST AND NECK (REMEMBER THE FRONT OF THE GOWN IS NOW CONTAMINATED)
STEP 5: GRAB THE INSIDE OF THE GOWN ONLY AND PULL GOWN AWAY
STEP 6: FOLD AND ROLL GOWN AND DISCARD
WHERE SHOULD HEALTHCARE PROFESSIONALS WEAR PROTECTIVE GARMENTS?
- HOSPITALS
- HOME HEALTH AIDE AGENCIES
- HOSPICES
- LONG-TERM CARE FACILITIES
- FIRST RESPONDERS
- NURSING HOMES
- PRIVATE HEALTHCARE CLINICS
Citations:
https://www.astm.org/COVID-19/
https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html
https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover.html
https://www.cdc.gov/HAI/pdfs/ppe/PPEslides6-29-04.pdf
https://www.cdc.gov/hai/pdfs/ppe/ppeposter148.pdf
https://www.cdc.gov/hai/pdfs/ppe/ppeposter148.pdf
https://www.cdc.gov/infectioncontrol/basics/transmission-based-precautions.html
https://www.cdc.gov/niosh/npptl/topics/protectiveclothing/default.html
https://www.cdc.gov/niosh/npptl/hospresptoolkit/training.html
https://www.cdc.gov/niosh/npptl/topics/protectiveclothing/default.html#table6
https://www.cdc.gov/oralhealth/infectioncontrol/faqs/personal-protective-equipment.htm
https://wwwn.cdc.gov/PPEInfo/Standards/Info/ANSI/ISEA1012014
https://wwwn.cdc.gov/PPEInfo/Standards/Info/ANSI/AAMIPB70Class3
https://www.cdc.gov/vhf/ebola/healthcare-us/ppe/guidance.html
Http://www.fda.gov/medical-devices/personal-protective-equipment-infection-control/medical-gowns
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4791533/
https://www.who.int/news-room/q-a-detail/q-a-coronaviruses
Zayba Syed is a graduate of Virginia Polytechnic Institute and State University working to pursue a Masters of Public Health-Physician Assistant (MPH-PA) dual degree.