Despite the availability of vaccines, we should continue masking to prevent the spread of COVID-19 until more people are vaccinated. In this article, Get Us PPE looks at different masking options and when each option is appropriate.

Editor’s note: After the time of publishing, the CDC updated their recommendations for fully vaccinated individuals, and additionally posted updated recommendations for all individuals.
___
In January 2021, the Center for Disease Control (CDC) issued an order for required masking on all public transport systems and in major transportation hubs, but masking had already been promoted for months as a general method to control the spread of COVID-19.
Wearing masks helps to protect the wearer and also prevents spread. Studies have shown that universal masking policies have been linked to lowered death/diagnosis rates in multiple communities.
However, there are many types of masks on sale in the marketplace, ranging from medical-grade to homemade masks. Most of these masks can be used by the general public; however, different scenarios require different levels of protection.
Below, we’ve compared different types of masks so that you know when to wear what and how to keep everyone as safe as possible!
Cloth Masks: Everyday masking for the average American
As surgical masks and N95s were quickly set aside for healthcare and frontline workers at the beginning of the pandemic, cloth masks sprung up as an affordable and easy-to-obtain alternative masking option to prevent COVID-19.

According to the CDC, “[c]loth masks not only effectively block most large droplets (i.e., 20-30 microns and larger) but they can also block the exhalation of fine droplets and particles (also often referred to as aerosols) smaller than 10 microns”. In addition, “[c]loth masks are comparable to surgical masks when used together for community control (i.e., when combined for both source control and personal protection.)” For these reasons, the World Health Organization (WHO) recommends the general public wear these in most circumstances.
Although some claim that cloth masks are ineffective, studies have shown otherwise. In a National Institute for Occupational Safety and Health (NIOSH)/CDC approved study on the effectiveness of different types of masks in blocking exhaled aerosols, a cloth mask was shown to be able to block a significant amount more than the single-layer gaiter and almost on par with a double-layer gaiter.
Ideally, cloth masks should be made of layers of tightly woven fabric that block light when held up to one and have a nose wire to conform to the shape of your face. Exhalation valves are discouraged as they are counteractive to the mask’s purpose, by allowing aerosols to escape. The WHO also warns against claims of “antimicrobial performance” as they are treated with chemicals that could potentially prove harmful.
3-ply masks are favored, meaning that they have three layers (or more) in the following order:
- an innermost layer of hydrophilic material (absorbent) – e.g., cotton
- a middle non-woven hydrophobic layer (helps to enhance filtration and retain droplets) – e.g., polypropylene
- an outermost layer of hydrophobic material (non-absorbent, limits droplets from escaping or getting in) – e.g., polyester/a polyester blend
To take care of reusable cloth masks, it’s recommended that you wash them daily with soap and hot water.
Surgical Masks: An extra layer of protection for those who need it most
Surgical masks are a common masking option to prevent COVID-19; these are disposable and typically come in blue with white straps. They are made of multiple layers composed of paper and plastic and should have a nose wire to be more form-fitting.
 According to the FDA, “a surgical mask is meant to help block large-particle droplets, splashes, sprays, or splatter that may contain germs (viruses and bacteria), keeping it from reaching your mouth and nose. Surgical masks may also help reduce exposure of your saliva and respiratory secretions to others.” Due to their loose-fitting nature, they are not considered “respiratory protection” as they filter more particles exhaled than inhaled.
According to the FDA, “a surgical mask is meant to help block large-particle droplets, splashes, sprays, or splatter that may contain germs (viruses and bacteria), keeping it from reaching your mouth and nose. Surgical masks may also help reduce exposure of your saliva and respiratory secretions to others.” Due to their loose-fitting nature, they are not considered “respiratory protection” as they filter more particles exhaled than inhaled.
The WHO recommends that surgical masks be worn by medical workers, those who have symptoms of COVID-19 (including those who are awaiting test results), those taking care of people suspected/confirmed to have COVID-19, people aged 60+/with underlying medical conditions, and anywhere where social distancing cannot be maintained. The CDC similarly suggests that surgical masks be worn anytime you are indoors or outdoors with those you don’t live with (not in your “bubble.”)
Ideally, surgical masks should be 3-ply as well and have an inner lining with moisture-wicking and anti-bacterial properties. When worn, they should be colored-side out, and as they are disposable, they should be discarded after a single use or if the mask has moisture, as that makes the mask ineffective. There are several ways to improve the fit of your surgical mask as well, including mask fitters, double masking, and knotting the ear loops (which will be discussed later.)
KN95 Respirators: The alternative to N95s for healthcare and frontline workers
KN95 respirators, like the more commonly known N95 respirators in the US, are a form of filtering respirators, which means that they are intended to prevent inhalation of particles or droplets.
This mask, which is typically white and in a conical No. 2 coffee-filter shape, has become a common option for those seeking alternatives to N95s reserved for frontline workers, but are still looking for high-level protection. The majority are produced in China, where a surge in domestic and international demand has led to a significant increase in manufacturers of KN95s.
However, that jump in production has been accompanied by a jump in the number of fake KN95s being sold.
For consumers, it is difficult to differentiate between real and imitated markings of certification. Respirators must achieve >95% efficiency in evaluations by NIOSH to qualify for medical use. Still, tests run by the National Personal Protective Technology Laboratory (NPPTL) have shown that several types of marketed respirators are unable to achieve the appropriate protective threshold (a full list of NPPTL assessments by the manufacturer can be found here). The CDC has estimated that around 60% of KN95s being sold are counterfeit.
The CDC also advises that KN95s should not be worn by those with large amounts of facial hair or anyone who finds difficulty breathing with the mask on. KN95s should also not be worn with other types of masks or layered for double masking purposes due to a hazardous reduction to breathability.
Clear Masks: A mask for the hearing impaired
Clear masks are important for those who are hard of hearing or deaf, as they rely on lip-reading to understand what people are saying, and masks prevent them from being able to do so. If you are interacting with people who are hearing impaired (or even just want people to see your face), CDC recommends the clear mask alternative.
Essentially, it is a typical cloth or surgical mask with a clear plastic panel sewn into the front that allows people to see your mouth. According to Main dans la Main, a French organization supporting those with hearing impairment, “they are also very useful for autistic people, people with learning difficulties and small children who might be scared of masks or need to be able to see facial expressions.”
When searching for suitable clear masks, medical experts emphasize that the plastic panel needs to be tightly sewn into the fabric to prevent leakage/openings and that it should still cover the nose, mouth, and chin like any other mask. In addition, some suggest searching for one with a nose rest because plastic does not conform to the face shape as easily as cloth. Having a nose rest will allow for a more fitted seal around the face and appropriate protection.
N95 Respirators: The healthcare worker’s mask
An N95 respirator is a single-use medical-grade “respiratory protective device designed to achieve a very close facial fit and very efficient filtration of airborne particles.” Due to their high effectiveness in filtering aerosols both exhaled and inhaled, the current CDC advice is that the general public does NOT wear N95s as “[t]hose are critical supplies that must continue to be reserved for health care workers and other medical first responders.”
The N95 shortage has been a constant since the beginning of the pandemic. According to Get Us PPE’s January Shortage Index, N95 masks were the third most requested type of PPE in January 2021, behind disinfecting wipes and nitrile gloves, and out of facilities in need of N95 masks in January, 86% were reusing N95s, often for a week or more. 53% of facilities requesting N95s had less than seven days’ supply remaining, and 28% had no supply at all. From an economics standpoint, the average cost of an N95 mask before the pandemic was $0.38 but now has risen up to $4-7 (a 1,300% increase.) Additionally, non-hospital facilities (long-term care clinics, nursing homes, acute-care facilities, schools, etc.) tend to pay more for N95s than large, wealthy hospitals because the latter are able to purchase N95s in bulk and negotiate better prices.
Manufacturers of N95s have been hesitant in trying to meet the demand. University of Notre Dame professor Kaitlin Wowak states that the production of N95s is determined by three factors: “the complexity of the equipment used to make the product, the availability of raw materials, and the availability of trained workers.” Due to the high financial investment required in each of these fields, makers were unwilling to immediately purchase the machines or materials required to up their output levels for fear that they would become wasted post-pandemic.
Separately, the rise of counterfeits on the market has contributed to the ever-present shortage as well. According to the president of Shepard Medical Products, Chris Humbert, “many new upstarts tried to sell him products billed as N95s, but because he couldn’t verify their quality or efficacy, he decided it would be safer to remain out of stock.” However, as approved manufacturers have begun investing in expanding their production levels, some are beginning to have surpluses, which, in addition to a focus on reaching underserved facilities, will hopefully help in bringing the nation out of its current PPE crisis.
How to Improve Your Mask’s Efficacy
To improve the effectiveness of a mask in blocking both exhaled and inhaled particles, experts have suggested various methods, including wearing a mask fitter, double masking, and tying mask loops.
A mask fitter is a flexible frame that can be worn on top of an existing mask. They help to reduce leakage by pressing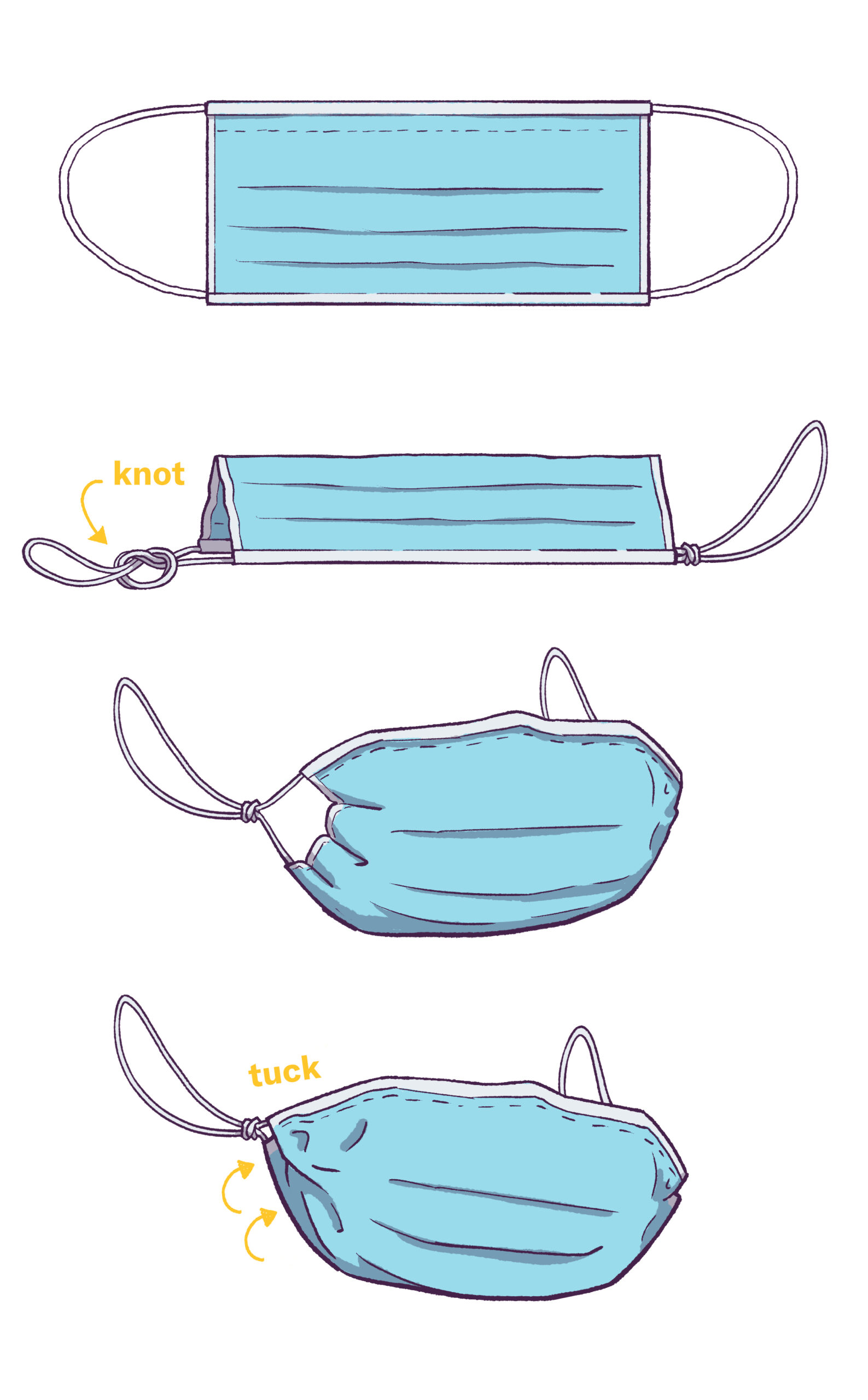 the mask more closely to one’s face. Various laboratories, such as Bellus 3D and the University of Wisconsin-Madison, have begun using 3D printing technology to produce these, and the former also provides 3D scanning technology in order to customize the fitter to the shape of one’s face for optimal fit and make masking more effective in preventing COVID-19.
the mask more closely to one’s face. Various laboratories, such as Bellus 3D and the University of Wisconsin-Madison, have begun using 3D printing technology to produce these, and the former also provides 3D scanning technology in order to customize the fitter to the shape of one’s face for optimal fit and make masking more effective in preventing COVID-19.
Another easier recommendation is to knot the loops of a surgical mask. Doing so helps to minimize the openings on the side of the mask, which in turn reduces leakage of aerosols and provides better protection (as seen in the image to the right.)
A final option is double masking. According to the CDC, “Wearing a second mask on top of a first mask (to create a “double mask”) can [i]mprove fit by pressing the inner mask closer to the face, thereby reducing the amount of air that leaks around the edges of the masks, [as well as] improve filtration by adding more layers of material to reduce the number of respiratory droplets containing the virus that come through the masks.” With the advent of a mutated strain of COVID-19 that is more contagious, health organizations have begun recommending double masking to further control the spread.
Cloth masks and surgical masks are not intended to be doubled-up on each other. Instead, it’s suggested that you layer a cloth mask on top of a surgical mask for optimal results.
Studies have shown that the previous layering description is effective in blocking aerosols in both directions. A CDC study noted that medical procedure masks, cloth masks, a double layer of cloth on a medical mask, and a knotted surgical mask respectively blocked 56.1%, 51.4%, 85.4%, and 77.0% of exhaled aerosols.
For inhaled aerosols, the following statistics were recorded for the percentage reduction in exposure, in comparison to an unknotted procedure mask:
| double mask | knotted mask | |
| transmitter masked
receiver unmasked |
82.2% | 62.9% |
| transmitter unmasked
receiver masked |
83% | 64.5% |
| both masked | 96.4% | 95.9% |
All of these alternative methods can help improve your mask’s efficacy, helping to keep yourself and those around you safe.
Why You Should Continue Masking to Prevent COVID-19
Even as vaccinations are rolling out, it’s still important that we continue masking to prevent COVID-19, as some states have seen increased cases after mask mandates were lifted. A study from the University of Washington projected that even with vaccinations if people relax on social distancing and masking, COVID-19 infections and death rates could increase. We also have not achieved herd immunity yet through vaccinations.
But for us to return to the “normal” that we are hoping for, we must continue masking when indoors to prevent yet another potential wave of the virus.